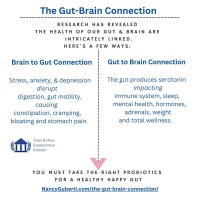
The connection between the gut and the brain, often called the gut-brain axis, is a complex and bidirectional communication system that influences various aspects of health, including mental well-being.
Here’s how these two seemingly remote areas of the body interact and the significant role of gut bacteria in this relationship:
Physical Connection: The Vagus Nerve
The brain physically connects to the digestive system through the vagus nerve, the longest of the twelve cranial nerves. This nerve links the intestines’ enteric nervous system (ENS) to the central nervous system (CNS). The ENS, also known as the “second brain,” is a vast network of neurons in the gut that controls digestive processes and operates independently of the Central Nervous system. However, it communicates with the CNS via the vagus nerve. This nerve is crucial for regulating unconscious bodily functions such as heart rate and digestion.
The human gut microbiome, which consists of trillions of bacteria, fungi, and other microorganisms, plays a crucial role in many aspects of health, including mental health and cognitive function.
Gut-Brain Axis
The gut-brain axis is a bidirectional communication system between the gut and the brain. This system includes neural, hormonal, and immune pathways through which the gut microbiome can influence brain function and mental health.
- Neural Pathways: The vagus nerve is a significant component of the gut-brain axis, transmitting signals from the gut to the brain. Certain gut bacteria can produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), affecting mood and behavior.
- Hormonal Pathways: Gut bacteria can influence the production of hormones that affect mood and stress responses. For instance, cortisol, the stress hormone, can be modulated by the gut microbiome.
- Immune Pathways: The gut microbiome plays a crucial role in regulating the immune system, which can impact brain function. Inflammation is caused by an imbalance in the gut microbiome (dysbiosis) linked to mental health conditions like depression and anxiety.
Cognitive Function
Studies have shown that the gut microbiome can affect cognitive functions such as memory, learning, and decision-making. For example:
- Probiotics: Certain strains of probiotics called beneficial bacteria improve cognitive functions. For instance, Lactobacillus and Bifidobacterium strains reduce symptoms of anxiety and depression.
- Diet: Diet influences the gut microbiome composition. Diets high in fiber and fermented foods can promote a healthy gut microbiome, supporting better cognitive function and mental health.
Mental Health Treatments
There is growing interest in using microbiome-based therapies to treat mental health conditions:
- Probiotic Supplements: Clinical trials are investigating the efficacy of probiotic supplements in treating depression, anxiety, and other mental health disorders.
- Prebiotics: Prebiotics are non-digestible fibers that promote the growth of beneficial gut bacteria. They can potentially treat mental health conditions by supporting a healthy microbiome.
- Psychobiotics are a class of probiotics specifically targeting mental health by producing neurotransmitters or reducing inflammation.
Research and Future Directions
Ongoing research aims to understand better the mechanisms through which the gut microbiome influences mental health. This research includes identifying critical bacterial strains, understanding how they produce neuroactive compounds, and developing targeted microbiome-based interventions.
Role of Gut Bacteria
Gut bacteria release chemical messengers that influence responses along the vagus nerve, effectively communicating with the brain. Our microbial interactions play a significant role in mental health and are implicated in various conditions:
- Mental Health Disorders: Research suggests a connection between gut microbiota and mental health disorders like Parkinson’s disease, depression, and bipolar disorder (BD). For instance, BD patients often show different gut microbiota compositions compared to healthy controls, with higher levels of certain bacteria correlated with more severe depression symptoms.
- Probiotics and Psychobiotics: Probiotics, beneficial live bacteria, are being studied for their potential to alleviate depression and anxiety. The term’ psychobiotics’ refers to probiotics that confer mental health benefits when ingested in sufficient quantities. This emerging field suggests modifying the gut microbiome could be a natural intervention for mental disorders.
Dietary Influence
Diet plays a crucial role in shaping our gut microbiome. The types of foods consumed can be toxic or medicinal, promoting the growth of beneficial bacteria or harmful pathogens. For example, diets high in sugar and fat can negatively affect gut health, while diets rich in fiber and fermented foods can enhance it. Additionally, research into vitamin D suggests it may help with Seasonal Affective Disorder (SAD), highlighting another way diet and gut health intersect with mental health.
Microbiota and Personality
Emerging studies suggest that gut bacteria influence behavior and memory, potentially affecting personality traits. For instance, some pathogenic bacteria can induce cravings for sugary foods, impacting mood and behavior. Research on toddlers has shown that gut bacteria can significantly affect mood, indicating that gut health might play a role in behavioral development.
Conclusion
The gut-brain connection underscores the importance of maintaining a healthy gut microbiome for overall well-being, particularly mental health. This relationship suggests potential for new treatments that involve modifying the gut microbiome through diet, probiotics, and other interventions. As research progresses, gut-brain probiotics may become a mainstream approach to managing and supporting mental health, offering alternatives to traditional pharmaceuticals.
It’s vital to your total wellness of mind and body and your longevity to keep your gut-brain health at its optimal state.
Unfortunately, conventional labs and doctors cannot offer the most insightful labs. An imbalanced gut microbiome can lead to various chronic digestive ailments and diseases, including autoimmune diseases.
The only way to gain a comprehensive snapshot of what’s going on in your gut and brain axis is to order a Comprehensive Stool Analysis.
This test will show you the health of your gut functioning, motility, digestion, and absorption and which beneficial bacteria strains your body needs most. The test detects root causes of acute or chronic illnesses that stem from the gastrointestinal tract, with correlations to disease states and health risks, to help you address chronic ailments and develop personalized solutions. The lab test includes a robust panel of pathogenic bacteria, yeast, viruses, and parasites known to cause serious health concerns in humans so that you can have a comprehensive view of potential health threats. It is the only method to gain personalized recommendations.
With healthcare, you get what you pay for, and conventional medicine labs are antiquated and focused on reactive, not proactive, or longevity purposes.
The question comes down to whether or not you are worth the investment in your wellness.
Tags: anxiety, comprehensive stool analysis test, deprssion, functional medicine labs, gut health, gut-brain axis, IBD, IBS, mental health, Nancy Guberti, vagus nerve
Leave A Reply (No comments So Far)
No comments yet